FINAL MASTERS PROJECT:
How might we redesign the interaction and delivery of the annual asthma review for patients with well controlled asthma.
RCA GROUP: Ally Rosam, Jieun Lee
The Brief:
The final self-directed project of our Masters Programme gave us the freedom and flexibility to choose the focus of our project based on our interests. We chose to focus on healthcare with a particular focus on transitional moments between physical and digital interactions.
The Design Problem:
The focus of the project was to redesign the health review for people with long-term conditions in the UK, due to the high prevalence (20% of the UK population ) and the huge cost that this group creates for the NHS (70% of the total health and social care budget). Patient demands for GP services are continuing to grow and patients are presenting with ever more complex complaints, whilst GP’s are facing mounting challenges around recruitment and retention.
The NHS has set out its priorities for the next 10 years, which includes its commitment to increasing support for helping people to manage their own health, which has shown to have benefits for both the individual and the healthcare system as a whole. This is particularly important because despite the aforementioned high costs, people with long-term conditions are actually spending the majority of their time managing their own health and wellbeing outside of a clinical setting.
Having explored the landscape of long-term conditions we decided to focus on asthma and use it as a case study. We discovered that most of the pain points were during the annual asthma review and that people don’t place much value on it. They consider it to be a waste of time as they are not learning anything new, it is an inconsistent experience in terms of both delivery and content, it often isn’t collaborative and they frequently feel like the HCP doesn’t fully understand their condition. From the perspective of the HCP there are high did not attend rates, time constraints, poor patient preparation as well as only providing a snapshot of how a patient is managing despite the variable and intermittent nature of the condition. Because of the poor experience during the review, the cycles of ‘before’ and ‘after’ within the self-management phase remained the same and were repeated every year.
The Barriers:
We didn't have a client and therefore narrowing down the focus of the project was challenging. Accessing patients and healthcare professionals was difficult and people weren't willing to talk openly about their health in groups. Therefore, although conducting in-depth one-to-one interviews was much more time consuming we believe that the quality of the insights gathered was far greater.
The Process:
We initially conducted desk based research, which we validated and explored further through in-depth interviews. We spoke to patients well as organisations who are involved in their care. We also did some early and rapid prototyping with paper and digital mock-ups and tested with patients with different long-term conditions, as a tool to try to explore what might be helpful in relation to effective self-management.

Testing prototypes

Validating tech feasibility
We analysed the conversations, identified emerging and recurrent themes related to self-management and mapped the journey that people go through during the early stages of their condition, until they finally reach self management. From the insights we also created a model of effective self-management, which was made up of four key components: Behaviour, Skills, Relationships and Adherence to the treatment regimen. We hypothesised that if all four components were in place then a patient was in a good position to effectively self manage their condition.
In order to explore the specific challenges around self management in relation to asthma, we identified the relevant stakeholders and conducted a second round of in-depth interviews. We subsequently ran a design sprint developed and tested the service with two patients in a small workshop, whereby we validated the benefit of the service to the patient as well as talking them through a wireframe of the service. We took a similar approach with GP’s, Community Pharmacists and CCG’s. In response to the feedback we made changes and iterated on the design. We also tested the service over one week with a lady with asthma, testing all of the key functionality via text message, to try to understand the content, language and frequency of the messaging.
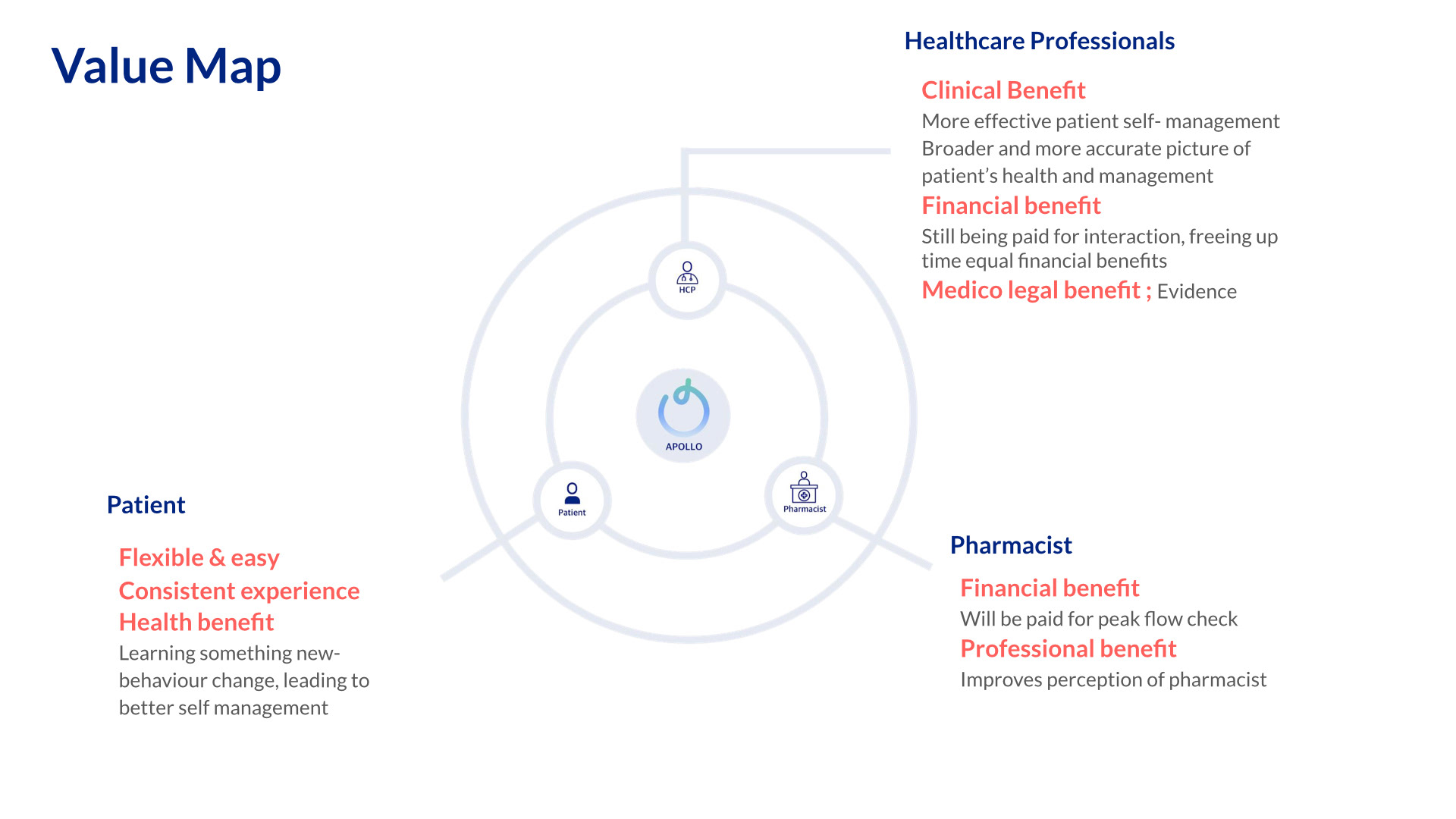
The Output: Apollo is the new flexible and easy way to carry out a health review, which gives a patient a broader and more accurate picture of how they are managing their health. It is a digital app that has been designed in the first instance for asthma patients with well controlled symptoms, that helps them to take greater ownership of their health, whilst reducing pressure on Primary Care.
Apollo uses the annual asthma review as a case study to showcase how the service could change patients’ experience of one component of General Practice through promoting greater self-management. The learnings from which could potentially be applied to other health reviews.
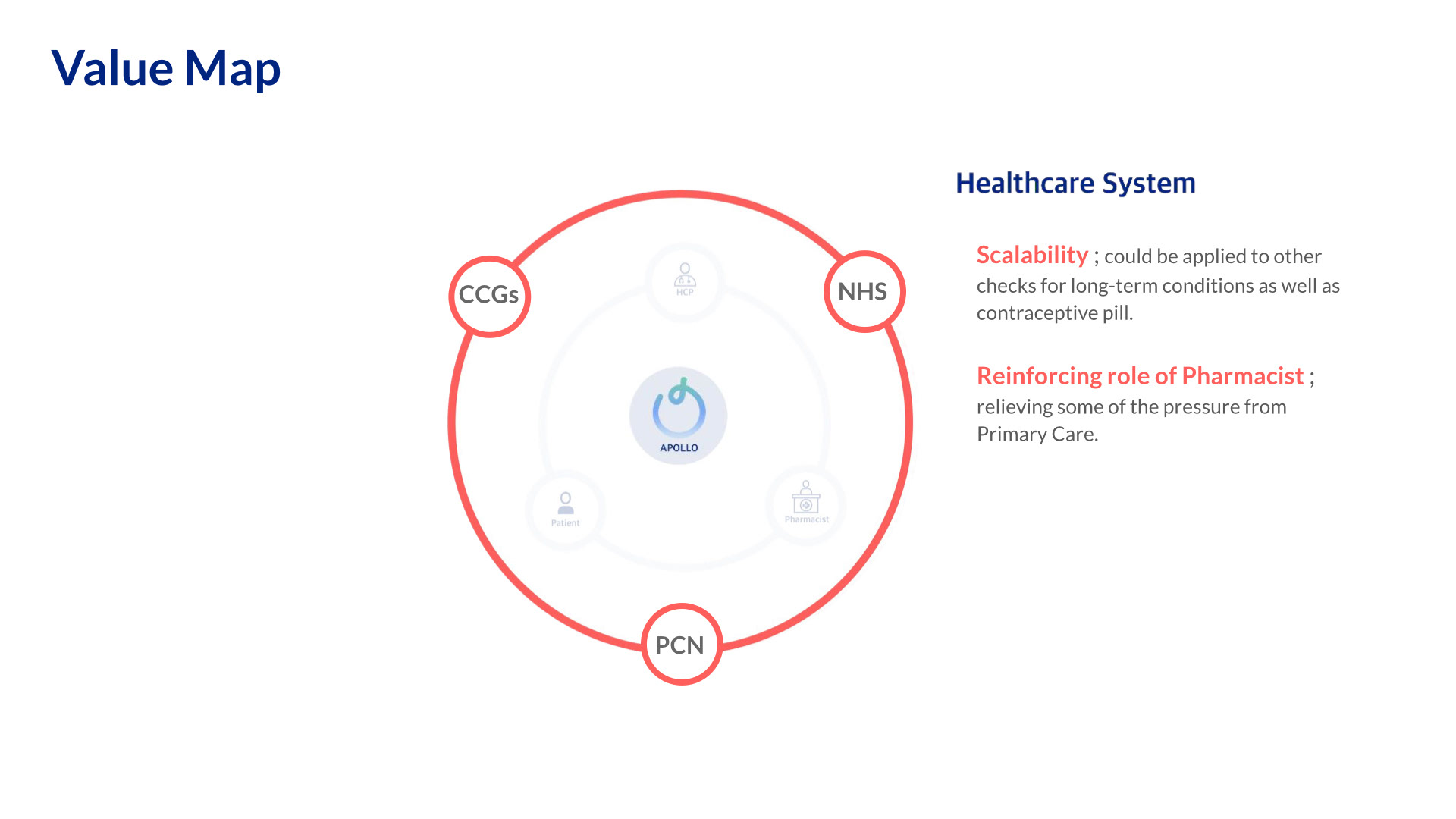
Apollo is different to the current annual asthma review, as it extends the moment by collecting the same information four times per year. There are also multiple other digital and physical touchpoints with the service, and it seeks to utilise existing physical interactions by reinforcing the role of Community Pharmacists.
We created a service blueprint in order to understand the front and back end requirements, which also highlighted areas that we had not considered; such as what to do if something goes wrong and when someone exits the service.
We created a business plan and considered how Apollo fits into the current ecosystem as well as how the data would be integrated with current healthcare systems in use within Primary Care.
We considered the market and calculated the section that Apollo could capture: There are 450,000 adults with well controlled asthma who are currently attending reviews, which is a conservative estimate and doesn’t take into account those who do not attend. Based on this section of the market Apollo could save the NHS time and money. It could free up 150,000 clinical hours, which is the equivalent of 450,000 HCP appointments, or considering it from another perspective it represents £13.5 million in time saved. In terms of measurement, the success of the service could be measured through higher attendance rates for reviews across all health conditions, a reduction in did not attend rates, fewer unplanned hospital admissions as well as greater and richer data capture.